Greater than 6 million folks use paid long-term providers and helps (LTSS) delivered in dwelling and community-based settings and greater than 2 million folks use LTSS delivered in institutional settings, in response to CBO estimates. LTSS embody the broad vary of paid and unpaid medical and private care providers that help with actions of day by day residing (similar to consuming, bathing, and dressing) and instrumental actions of day by day residing (similar to making ready meals, managing treatment, and housekeeping). The 8 million folks utilizing LTSS solely consists of folks requiring ongoing or upkeep remedy. Many others use comparable providers on a shorter-term or intermittent foundation, similar to care offered via the Medicare dwelling well being and expert nursing facility advantages. Direct care employees play a pivotal function in offering these providers. They carry out demanding, high-stress work for low wages and sometimes no advantages.
This evaluation makes use of the 2022 American Group Survey to offer an outline of demographic traits, wages, and medical insurance protection of direct care employees, which embrace dwelling well being aides, private care aides, nursing assistants, licensed sensible nurses (LPNs), and registered nurses (RNs). It focuses particularly on direct care employees in nursing amenities, residential care amenities, and residential well being in addition to those who present providers or work in settings that present nonresidential providers for older adults and youthful adults with disabilities (see Strategies). In doing so, we study the direct care workforce broadly and variations throughout job classifications and settings of labor. Key takeaways embrace:
There are almost 3 million direct care employees who’re predominantly feminine (87%) and low-wage (65%); over one-quarter are Black (28%) and over 4 in ten are 50 years previous or extra (41%) (Determine 1).
Direct care employees work throughout quite a lot of settings and embrace private care aides, nursing assistants, dwelling well being aides, LPNs, and RNs (Determine 2).
Dwelling well being aides, private care aides, and nursing assistants (collectively, “aides”) and LPNs usually tend to be beneath 35, Black or Hispanic, low-wage employees, uninsured, or lined by Medicaid compared with RNs (Determine 3).
Nursing amenities and residential care amenities have larger shares of nurses (LPNs and RNs) when in comparison with dwelling well being settings and providers for older adults and youthful adults with disabilities (collectively, “dwelling and community-based settings”) (Determine 4).
Direct care employees in dwelling and community-based settings usually tend to be noncitizens and work part-time when in comparison with these in nursing amenities and different residential care settings (Determine 5).
There have been longstanding challenges discovering sufficient employees to offer LTSS for individuals who want such providers, and the COVID-19 pandemic exacerbated these points significantly. In a 50-state survey of officers administering Medicaid HCBS applications, almost all responding states reported they have been experiencing shortages of direct help professionals, private care attendants, and/or dwelling well being aides. The adequacy of staffing in nursing amenities has additionally been a longstanding concern.
In response to workforce points, the federal and state governments have taken motion to help direct care employees. Part 9817 of the American Rescue Plan Act (ARPA) offered states with a further 10 proportion factors of federal funding for his or her Medicaid HCBS expenditures that occurred between April 1, 2021, and March 31, 2022. States have been required to reinvest the extra federal funding in Medicaid HCBS, leading to an estimated $37 billion of latest HCBS funding. As of December 31, 2023, the primary use of the ARPA funds—accounting for greater than $26 billion of the deliberate $37 billion in new funding—was for workforce recruitment and retention. The second largest use (a further $4 billion) was for workforce coaching. Different makes use of of funding embrace high quality enchancment actions and decreasing or eliminating HCBS ready lists.
The Biden-Harris Administration finalized two guidelines aimed toward addressing shortages of direct care employees: (1) the first-ever necessities for nurse staffing ranges in nursing amenities, and (2) a rule governing entry to Medicaid providers with a number of provisions to strengthen the HCBS workforce, together with requiring states to spend least 80% of whole Medicaid funds for sure HCBS on compensation for direct care employees, a provision that won’t take impact till 2029. Many states have adopted cost price will increase for HCBS suppliers and nursing amenities with the purpose of boosting staffing ranges, as reported to KFF in a 2023 survey. Vice President Harris additionally just lately put forth a proposal that may set up a brand new Medicare dwelling care profit, amongst different adjustments. Though the proposal doesn’t but have specifics, it proposes enhancements for care employees through entry to higher wages.
In 2022, there have been almost 3 million direct care employees who offered LTSS to folks ages 65 and older and other people beneath 65 with disabilities. These employees have been predominantly feminine (87%) and low-wage (65%); over one-quarter have been Black (28%) and over 4 in ten have been age 50+ (41%) (Determine 1). Almost one in three have been part-time employees, and about one in ten have been noncitizens, uninsured, and/or lived in rural areas. These demographic traits are all considerably extra widespread amongst direct care employees than amongst different working adults (Appendix Desk 1).
Field 1: Who Are Direct Care Employees and The place Do They Work?
By Kind of Employee:
Dwelling Well being Aides: Dwelling well being aides help older adults and other people with disabilities residing at dwelling with medical care. They could assist with checking important indicators, help with medical gear, and assist with administering treatment. They could additionally assist with actions of day by day residing (ADLs), which embrace consuming, bathing, dressing, aiding with strolling/train, and utilizing the lavatory.
Private Care Aides: Private care aides help older adults and other people with disabilities residing at dwelling with ADLs. Private care aides additionally assist with instrumental actions of day by day residing (IADLs), similar to grocery procuring, meal preparation, and managing medicines.
Nursing Assistants: Nursing assistants, or licensed nursing assistants (CNAs), sometimes work in nursing houses and help residents with ADLs. All CNAs will need to have accomplished a nurse aide coaching and competency analysis program inside 4 months of their employment. They need to additionally pursue persevering with schooling every year.
Licensed Sensible Nurses (LPN): LPNs present care beneath the course of a registered nurse (RN). Collectively, RNs and LPNs make sure that somebody’s plan of care is being adopted and their wants are being met. LPNs sometimes have one yr of coaching.
Registered Nurses (RN): RNs are liable for the general supply of care and assess total well being care wants. RNs are sometimes required to have between two and 6 years of schooling.
By Setting of Care:
Nursing Amenities: Nursing amenities are residential settings that present round the clock nursing and private care to residents who both want short-term rehabilitation following a hospitalization or damage or long-term care to residents with persistent medical and/or psychological well being circumstances requiring entry to 24-hour expert care and help with ADLs or private care.
Residential Care Amenities: These settings embrace residential settings that serve people with mental and developmental disabilities, psychological sickness, or substance use dysfunction. These settings additionally embrace institutions that present residential and private care providers for older adults or youthful adults with disabilities who’re unable to totally take care of themselves. These settings can embrace assisted residing amenities, persevering with care retirement communities, and group houses for adults with disabilities. The care sometimes consists of room, board, supervision, and help with actions of day by day residing.
Dwelling Well being: Dwelling well being companies are organizations that present expert rehabilitative or post-acute care in addition to long-term private take care of sufferers. The identical expert providers offered by expert nursing amenities, similar to nursing, occupational remedy, and bodily remedy, are as a substitute offered within the dwelling, together with help with ADLs and IADLs.
Companies for the Aged and Individuals with Disabilities: These are providers or settings that present nonresidential, social help providers for older adults and youthful adults with disabilities. These institutions sometimes give attention to the welfare of those people in such areas as day care, non-medical dwelling care or homemaker providers, social actions, group help, and companionship. These providers and settings can embrace grownup day care facilities, dwelling care providers for older adults, and companion providers.
Direct care employees present care throughout numerous settings: 58% labored in dwelling well being settings or offered nonresidential providers for seniors and other people with disabilities (collectively, “dwelling and community-based providers” or “HCBS”), 29% labored in nursing amenities, and the remaining 13% labored in residential care amenities (Determine 2). Nursing amenities are probably the most medically-oriented institutional settings, offering each short-term expert nursing and long-term upkeep care providers. Residential care amenities embrace quite a lot of settings – some institutional and a few community-based – and are, as a bunch, much less institutionalized than nursing amenities. HCBS are offered in folks’s houses and different community-based settings (Field 1).
Over three-quarters (77%) of direct care employees have been private care aides, nursing assistants, or dwelling well being aides (collectively “aides”) and the remaining quarter (23%) have been registered nurses (RNs) or licensed sensible nurses (LPNs) (Determine 2). Direct care employee duties fluctuate, with some employees primarily offering private care providers, some offering primarily medical care, and a few offering a mixture of each. Aides have a tendency to offer principally private care providers whereas RNs present principally medical care, and LPNs present each sorts of providers (Field 1). The academic necessities for LPNs and, particularly, RNs, are larger than the necessities for aides on account of the extra medical nature of their duties.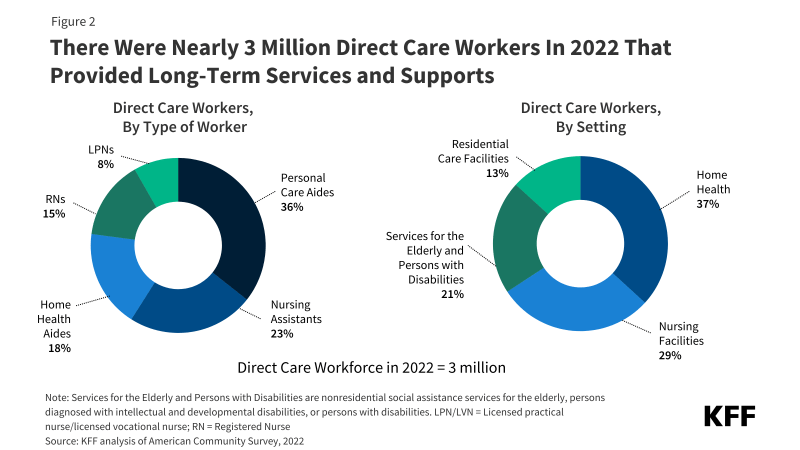
In contrast with registered nurses, larger percentages of aides and LPNs are youthful, Black or Hispanic, low wage, and lined by Medicaid or uninsured (Determine 3). Almost one in three aides (31%) and over one in 4 LPNs (27%) are beneath 35 years previous, in contrast with only one in 5 RNs (20%). Over half of all aides (52%) and almost 4 in ten LPNs (39%) are Black or Hispanic, in comparison with simply 25% of RNs. RNs are the very best paid direct care employees and aides are the lowest-paid direct care employees, with over three-quarters (76%) of aides reporting wages beneath $35,000. As compared, simply one-fifth (21%) of RNs report wages of lower than $35,000. LPNs’ wages are larger than these of aides however decrease than these of RNs. The variations in wages are probably attributable, at the least partially, to the truth that the academic necessities are most rigorous for RNs and least rigorous for aides. Aides are additionally extra probably than nurses to work part-time, probably one other contributing issue to the wage discrepancies (Appendix Desk 1). Aides are twice as more likely to be uninsured in contrast with RNs (12% vs 6%) and 4 occasions as more likely to be lined by Medicaid (35% vs 9%). LPNs are almost twice as probably as RNs to be uninsured (11% vs 6%) or be lined by Medicaid (16% vs 9%).
Nursing amenities and residential care amenities have larger shares of nurses in comparison with dwelling and community-based settings (Determine 4). The share of direct care employees who’re RNs or LPNs is 43% in nursing amenities, 21% in residential care amenities, and 14% in dwelling and community-based settings. The Biden-Harris Administration launched a rule that creates new necessities for nurse staffing ranges in nursing amenities, together with minimal ranges for nurse aides and registered nurses. This rule was extremely anticipated as it could create the first-ever federal minimal staffing ranges, although even previous to the staffing rule, many states had their very own minimal staffing ranges. In distinction, a brand new rule on entry to Medicaid providers consists of a number of necessities concerning the adequacy of states’ funds for direct care employees in dwelling and community-based settings, however doesn’t set up any minimal staffing ranges for such settings.
Direct care employees that work in dwelling and community-based settings are considerably extra more likely to be noncitizens, work part-time, and have decrease wages when in comparison with these in nursing amenities and different residential care settings (Determine 5 and Appendix Desk 1). Amongst direct care employees in dwelling and community-based settings, 12% are noncitizens in contrast with 8% in residential care amenities and 6% in nursing amenities. Noncitizens embrace those that are lawfully current in addition to those that are undocumented, although the vast majority of noncitizen immigrants are lawfully current. Half-time work can also be extra widespread amongst employees in dwelling and community-based settings, with 40% of employees working part-time in contrast with 22% of nursing facility employees and 24% of residential care facility employees. Direct care employees total usually tend to be part-time employees than all grownup employees (32% vs 16%), which can be a part of the rationale they’re extra more likely to have wages beneath $35,000 (64% vs. 38%) (Appendix Desk 1). Low wages amongst direct care employees broadly are a key driver within the excessive turnover within the workforce, which has spurred motion amongst federal and state policymakers. The Biden-Harris administration finalized a rule aimed toward making certain entry to Medicaid providers, which included a provision that requires states to spend least 80% of whole funds for sure HCBS on compensation for direct care employees. Most states have additionally elevated funds to direct care employees to extend the availability of HCBS employees, although a few of these states have indicated that a few of these will increase are momentary.
Each 2024 presidential candidates have addressed direct care workforce shortages of their occasion platforms, however questions stay about how the shortages could be addressed. The Republican platform proposals tackle disincentives that contribute to workforce shortages, however it’s unclear what insurance policies a Republican Administration would put forth to realize these objectives. On October 8, 2024, Vice President Harris put forth a proposal that may set up a brand new Medicare dwelling care profit, amongst different adjustments. Though the proposal just isn’t totally specified, it proposes to elevate up care employees by offering entry to higher wages. If enacted, the Harris proposal could be the primary main growth of Medicare for the reason that Medicare Modernization Act of 2003 that added a prescription drug profit to this system. Many coverage particulars must be labored out because the proposal wound its approach via Congress, together with questions on eligibility, profit design, financing, and workforce shortages.
Strategies
This evaluation relies on KFF evaluation of the 2022 American Group Survey (ACS), 1-year file. The ACS features a 1% pattern of the US inhabitants, and the subset of direct care employees used right here consists of over 26,000 observations. Direct care employees are those that fall into the next occupation codes: Registered nurses (3255); Licensed sensible and licensed vocational nurses (3500); Dwelling well being aides (3601); Private care aides (3602); and Nursing assistants (3603). Dwelling well being aides, private care aides, and nursing assistants are collapsed into “Aides” in components of this evaluation. This evaluation solely consists of those that work within the following industries: Dwelling Well being Care (8170), Nursing Care Amenities (8270), Residential Care Amenities (8290), and Particular person and Household Companies (8370). Dwelling well being care and particular person and household providers are collapsed into “HCBS” for components of this evaluation.
These industries seize the vast majority of employees offering long-term well being providers. They exclude some employees who could also be offering ongoing non-health social providers to people. The ACS asks respondents about their medical insurance protection on the time of the survey. Respondents could report having a couple of kind of protection; nonetheless, people are sorted into just one class of insurance coverage protection.
We outline the direct care workforce as all people who earned at the least $1,000 in the course of the yr and indicated that their job was in each the long run care trade and occupation codes listed above.
Notably, the ACS doesn’t embrace unpaid LTC caregivers, similar to kinfolk and pals, who really present the vast majority of community-based long-term providers and helps within the US. A limitation of federal surveys broadly, together with ACS, is the probably underrepresentation of noncitizens, notably current and undocumented immigrants.





















